A healthy man in his seventies developed left-sided tension pneumothorax with a decrease in oxygen saturation and blood pressure during shoulder arthroscopy on the same side. Perioperative ultrasound to examine lung sliding is a simple method for quickly identifying this rare but potentially dangerous situation.
A lung-healthy, 180 cm tall, non-smoking and physically fit man in his seventies underwent a two-hour arthroscopic repair of the rotator cuff in the left shoulder while in the right lateral position. No nerve block was applied, but 20 ml of local anaesthesia was injected into the shoulder joint before and after surgery. The patient received intravenous anaesthesia in the form of remifentanil and propofol, and a size 5 laryngeal mask was fitted without issue.
Monitoring included ECG, pulse oximetry, blood pressure and capnography. Ventilation was pressure-controlled with 9 cm of water, 40 % oxygen, and without positive end-expiratory pressure. Mean blood pressure remained stable at 70 mmHg, and oxygen saturation was 95–98 %.
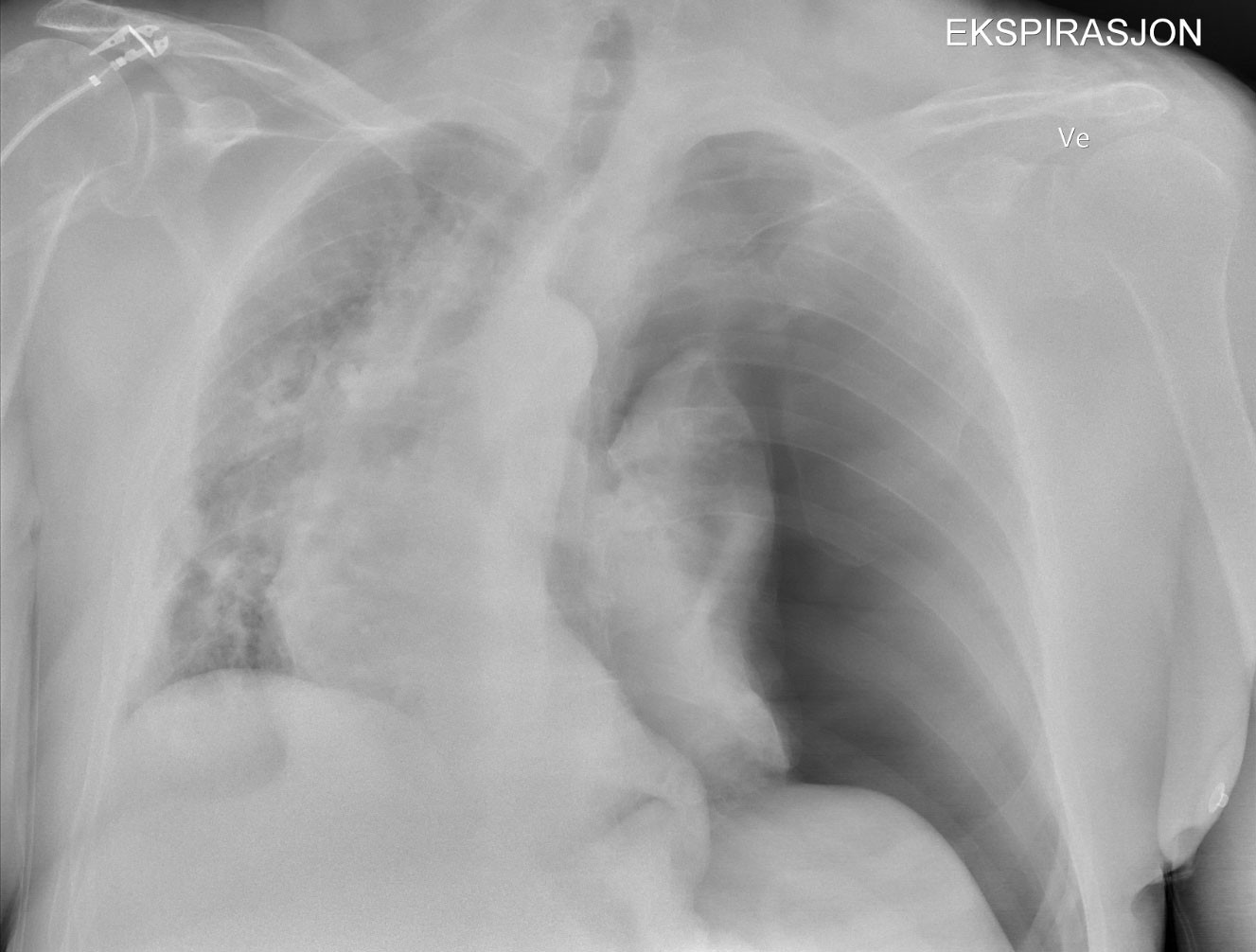
One hour before the end of the operation, oxygen saturation dropped to 89 %, tidal volume from 550 ml to 366 ml, and mean blood pressure from 70 mmHg to 60 mmHg. Oxygen in inspired air was increased from 40 % to 100 %, and inspiratory pressure was increased from 9 cm to 18 cm of water. Oxygen saturation rose to 91 % and blood pressure remained unchanged. No lung auscultation or blood gas analysis were performed. Surgery was completed, anaesthesia was stopped and the laryngeal mask was removed without difficulty. Upon arrival at the postoperative ward, oxygen saturation was 88 % despite the application of a non-rebreather oxygen mask. The patient was dyspnoeic, clammy and pale, with blood pressure of 90/60 mmHg. The duty anaesthetist was immediately called. In an ultrasound scan a few minutes later, the anaesthetist found an absence of lung sliding of the left pleural blades. Chest x-ray confirmed left-sided tension pneumothorax (Figure 1).
Under local anaesthesia, the surgeon placed a 12 French Portex chest drain in the fifth intercostal space in the operating room 1.5 hours after the shoulder surgery. The lung re-expanded after two hours with 5 mmHg suction. In the intensive care unit three hours after surgery, the patient needed pain medication, but his blood pressure had normalised and the oxygen supply was reduced from 6 L to 2 L via nasal cannula. The thoracic drain was removed after 15 hours, and the patient was discharged 24 hours after surgery. At the six-month check-up, he was symptom-free and active.
Discussion
Pneumothorax after shoulder arthroscopy is rare and is most often reported in case studies, with over 30 articles on PubMed describing cases during shoulder arthroscopy and up to ten hours postoperatively (1). It may therefore be that several minor, asymptomatic cases remain undetected, as 94 % of these resolve spontaneously (2).
Pneumothorax from the rupture of smaller bullae cannot be ruled out in our patient. However, it is unlikely that bullae that do not rupture during normal coughing, which can generate pressures of up to 400 cm of water (3), would rupture due to airway pressure of 20 cm of water under anaesthesia. Furthermore, ventilation during surgery was normal, and the patient never coughed with the laryngeal mask in place. The local anaesthesia administered by the surgeon in the shoulder joint probably did not reach the pleural cavity due to the distance, and diathermy was not used. Additionally, no interscalene nerve block was applied, which can cause pneumothorax, especially before an ultrasound scan (4).
The literature we have found indicates that the aetiology of pneumothorax during shoulder surgery is the surgery itself, as pneumothorax always occurs on the same side as the arthroscopy (5). Several cases of pneumomediastinum and subcutaneous emphysema without pneumothorax also suggest that the air originates from the arthroscopy, not from the lungs (6). In shoulder arthroscopy such as this, 3–5 ports are created in the skin for the arthroscope and surgical instruments. Suction and infusion pump pressures of 30–60 mmHg (41–82 cm water) are used with approximately 20 litres of 0.9 % NaCl irrigation solution.
'In terms of my experience of the situation, I must say that I hardly noticed the event itself and had no reactions afterwards.'
One possible mechanism is that the negative pressure from the arthroscopy pumps draws air through open working portals, alternating with positive pressure that pushes both air and water into the surrounding tissue of the shoulder joint (7). When the arthroscope is inserted and removed multiple times, air can also be drawn in, in the same way as a bicycle pump. Air can also enter the irrigation fluid via loose tube connections if the irrigation fluid bags are not changed in time and air enters the tubing, or if the soft tissues around the wound act as a one-way flap valve during shoulder movement (6). Irrigation fluid can also lead to hydrothorax (8). Air and water can follow fascial layers and channels into the pleural cavity, based on embryological and radiological findings (9).
Our patient history shows that shoulder arthroscopy can, in rare cases, lead to pneumothorax. Perioperative ultrasound to identify lung sliding is a simple method for quickly identifying and thus managing this potentially dangerous situation.
The patient has consented to publication of this article.
The article has been peer-reviewed.
- 1.
Bamps S, Renson D, Nijs S et al. Pneumothorax after Shoulder Arthroscopy: A Rare but Life-threatening Complication. J Orthop Case Rep 2016; 6: 3–5. [PubMed][CrossRef]
- 2.
PSP Investigators. Conservative versus Interventional Treatment for Spontaneous Pneumothorax. N Engl J Med 2020; 382: 405–15. [PubMed][CrossRef]
- 3.
Fontana GA, Lavorini F. Cough motor mechanisms. Respir Physiol Neurobiol 2006; 152: 266–81. [PubMed][CrossRef]
- 4.
Klaastad O, Sauter AR, Dodgson MS. Brachial plexus block with or without ultrasound guidance. Curr Opin Anaesthesiol 2009; 22: 655–60. [PubMed][CrossRef]
- 5.
Sun WC, Kuo LT, Yu PA et al. Pneumothorax, an Uncommon but Devastating Complication following Shoulder Arthroscopy: Case Reports. Medicina (Kaunas) 2022; 58: 1603. [PubMed][CrossRef]
- 6.
Van Nieuwenhuyse ESM, Kerens B, Moens J et al. Subcutaneous emphysema after shoulder arthroscopy. A case report and review of the literature. J Orthop 2017; 14: 287–9. [PubMed][CrossRef]
- 7.
Kateros K, Skotidis E, Bablekos GD et al. Pneumothorax After Shoulder Arthroscopy: A Rare Complication of Rotator Cuff Repair Surgery. Cureus 2023; 15. doi: 10.7759/cureus.36774. [PubMed][CrossRef]
- 8.
Connett B, Krohn EF, Hilu J. Complete Hydrothorax After Revision Shoulder Arthroscopic Surgery: A Case Report. Cureus 2022; 14. doi: 10.7759/cureus.23590. [PubMed][CrossRef]
- 9.
Lee SY, Chen CH, Sheu CY et al. The radiological manifestations of the aberrant air surrounding the pleura: in the embryological view. Pulm Med 2012; 2012. doi: 10.1155/2012/290802. [PubMed][CrossRef]